Aging populations should be embraced, not feared
The story of demographic doom has become familiar: Declining birth rates will cause populations to shrink, while longer lifespans will increase the costs of pensions and eldercare. Relatively fewer workers will have to pay for it all.
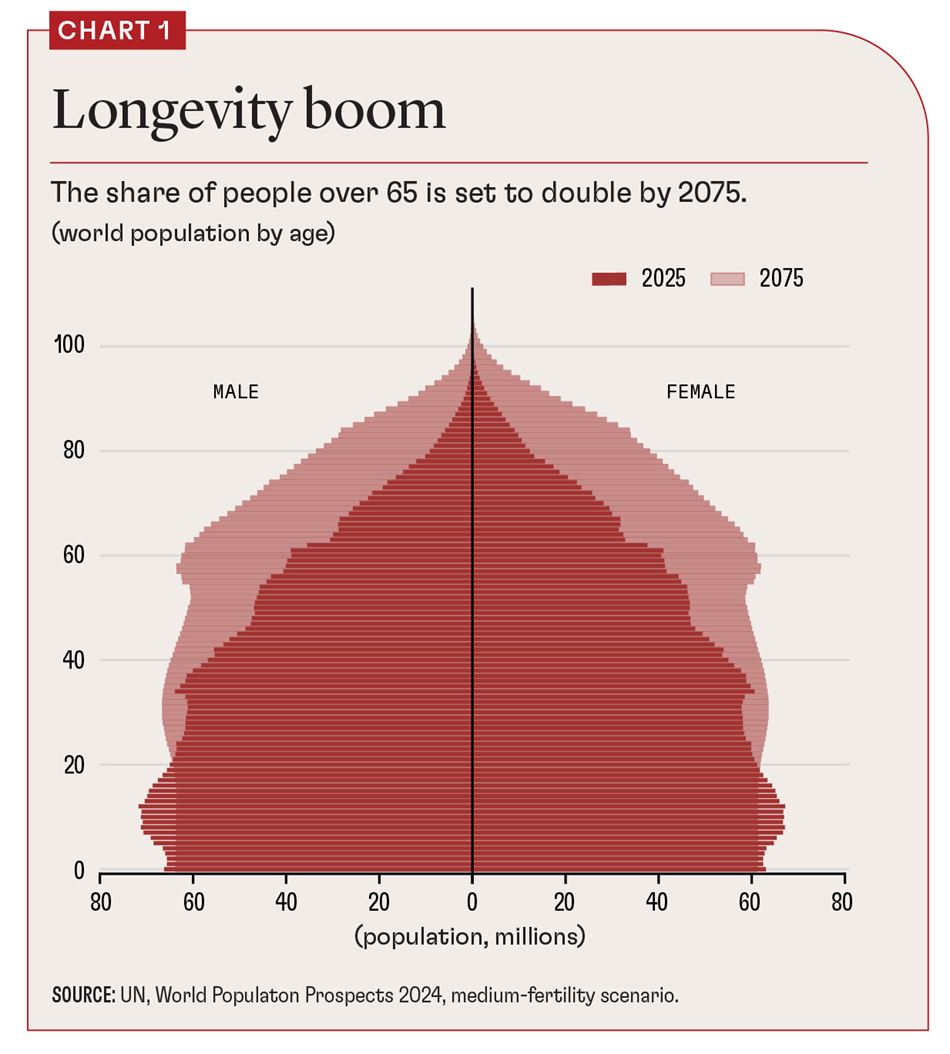
This story is partly true: One in ten people worldwide are now over 65, and that proportion is projected to double over the next 50 years (see Chart 1). Population decline has already begun in places such as Japan and China. Those countries are also experiencing a sharp increase in median age, as is Europe.
But the pessimism around an aging population is too one-sided. In fact, the combination of older people becoming more numerous and more likely to work makes them essential to economic dynamism.
In Europe, 90 percent of the increase in workers in the past decade—17 million more people in employment—came from a jump in workers over 50, according to the Organisation for Economic Co-operation and Development. In Japan, the proportion is even higher. In both places, older workers are already the main driver of GDP growth.
This is just one component of the “longevity dividend” societies can reap if we rethink our approach to aging (Scott 2024). It starts with reframing the policy debate in two fundamental ways.
The first is to stop seeing an aging society only as a problem. This is a strikingly negative way of framing one of the greatest achievements of the 20th century: Most of humanity is living longer, healthier lives. That’s an opportunity.
The second is to drop the unworkable focus on changing individual behavior in order to preserve current systems. Instead, focus on helping each person adapt to greater life expectancy—give them the support needed to live their best longer life.
This perspective points us to a new approach to aging based on redesigning health systems and investing more in our later-life human capital to seize the opportunities of an older, more experienced population.
Adapting to longevity
In the 20th century, more people living from 40 to 60 meant more years when people tended to be employed and in reasonably good health. In this century, life expectancy gains mean more people living from 60 to 90. If people’s behavior doesn’t change and systems are still based on the life expectancy of the previous century, pension and health costs will rise and be a drag on economies, especially those of richer countries.
For individuals, longer life causes a profound change in outlook. When there is only a small chance of living long enough to become old, investing to benefit your future octogenarian self doesn’t make sense. But with global life expectancy now exceeding 70, and even 80 in an increasing number of countries, it does.
This logic has radical implications for our health, education, work, and financial systems—areas where traditional approaches are no longer working.
Raising the state retirement age generates widespread resistance. Policies aimed at raising birth rates are expensive and have relatively modest effects because they go against individual preferences. Immigration holds political challenges.
What’s more, the latter two sets of policies target changing the relative size of different age groups but do not address the deeper challenge of how we adjust to longer lives. If longevity is what makes our pensions and health systems unsustainable, higher birth rates or immigration merely delay the financial day of reckoning.
Investing in the human and social capital of our later years is the only sustainable solution to the challenges of an aging society.
Expansion of morbidity
Gains in life expectancy over the previous century drove an epidemiological transition, with the health burden shifting from infectious to chronic noncommunicable diseases (Omran 1971). The latter now account for 60 percent of the disease burden globally, and 81 percent in the European Union.
Because of this shift in the disease burden, healthy life expectancy has not grown as fast as overall life expectancy, causing an expansion of morbidity. The current health system is at risk of keeping us alive but not healthier for longer, at an ever-increasing cost to individuals, families, and society.
In short, in the 20th century, we added years to life. In the 21st, we must add life to these extra years.
This requires a shift toward chronic disease prevention and health maintenance, not just treating people when they become ill. Three factors make the switch to prevention more feasible and desirable.
First, increased longevity means that most people can expect to experience chronic disease.
Second, the growing availability of structural risk and genetic data makes targeted interventions possible. Given the significant role of socioeconomic factors in driving health, this points to a clear link between reducing poverty and improving a country’s health as well.
Third, advances in biology hold the prospect of more effective forms of prevention. The dramatic impact of GLP-1 drugs such as Ozempic and Wegovy shows how a single class of therapeutics can help postpone the incidence of multiple diseases. Likewise, developments in the biology of aging hold the potential for future drugs that tackle aging-related diseases directly.
Increased investment in life sciences and biopharmaceuticals should lead to the development of these therapies, as well as to modes of prevention that work better and are more cost-effective. Promising areas include improved vaccines for older people that exploit potential gains in geroscience, cancer therapies, synthetic biology, and genomics.
Life-course approach
A focus on prevention demands many radical changes. If the aim is a healthy 90-year-old, a life-course approach to health should start in childhood—and no later than middle age. The next step is to make measures of healthy life expectancy a key metric in allocating health expenditure, rather than measuring output in terms of treating disease and performing operations.
Financing is a definite challenge. Health and social care costs are already rising in the European Union because of an aging population, so prevention entails additional spending. That means either more government debt or innovative financing, such as social impact bonds that support increased health expenditure today funded by future gains.
Significant improvements in life expectancy in the 20th century were the result of major innovations in health care, public health, and pharmaceuticals. Substantial gains in healthy longevity in this century will require the same.
As demonstrated in Japan, robotics can offer solutions for care, particularly when there are not enough nurses and support staff. Digital innovation and artificial intelligence also have great potential to fine-tune targeted personalized medicine and improve prevention—as long as we invest in digital literacy across all ages and social strata.
A shift from treating disease to focusing on health means tackling the many socioeconomic factors that impact health. Involvement of sectors beyond health care is needed, including businesses, all levels of government, communities, and the food and housing industries, to name a few.
This broader perspective supports policies such as taxing unhealthy foods and public health campaigns that encourage exercise and healthy living. Further, in a world of shrinking populations, tackling inequality will make increasing economic sense: Society must help all people make their fullest contribution.
Boosting employment
Nearly 90 percent of Europeans in their late 40s are in the labor force. But workforce participation falls below half by people’s early 60s, even as people are living longer and therefore spending more.
As a result, the policy debate understandably focuses on changes in the state retirement age. However, while raising the age helps the public purse, it does little to help individuals keep working longer.
Boosting employment from age 50 up requires a much broader range of policies across a wider range of ages. Areas of focus include health, skills, and the creation of age-friendly jobs.
With an aging population, health isn’t important just for individual welfare but for the entire economy. Someone diagnosed with cardiovascular disease at age 50 is 11 times more likely to leave employment in the United Kingdom.
Returning to work is especially difficult for older individuals, which means that preventive health policies provide substantial macroeconomic value. A 20 percent reduction in the incidence of six major chronic diseases increases GDP 1 percent within five years and 1.5 percent in ten years, thanks to higher labor force participation, evidence for the UK suggests (Schindler and Scott, forthcoming). The effect is most pronounced for workers ages 50 to 64.
But good health alone is not enough to keep people engaged in employment for longer. We also need the kinds of age-friendly jobs older people prefer—with more flexible hours, fewer physical demands, and greater autonomy. By reducing the competition between younger and older workers, such jobs limit the career impact on the former.
While age-friendly jobs are becoming more common, many occupations, such as construction, remain difficult for older workers. This highlights the need for policies to help with reskilling and transitions into new occupations throughout life, as well as anti-age-discrimination laws.
Such policies not only boost employment, they increase the efficacy of raising the state retirement age and offer a fairer social contract for adaptation to a longer life.
Demography isn’t destiny
The aging society narrative emphasizes that failure to adapt to longer lives carries the risk that we will outlive our health, wealth, relationships, and sense of purpose.
In 1951, the Welsh poet Dylan Thomas wrote a poem dedicated to his dying father, “Do Not Go Gentle into That Good Night,” urging that we fight death and push back against the inevitable. Similarly, we should not gently accept that demography is destiny.
How we age can be influenced by a host of individual actions and government policies. By making adaptation and adjustment to longer lives an urgent priority, we can deliver a three-dimensional longevity dividend of longer, healthier, and more productive lives.
Our future demands that we seize this opportunity.
Opinions expressed in articles and other materials are those of the authors; they do not necessarily reflect IMF policy.
References:
Omran, A. R. 1971. “The Epidemiologic Transition.” Milbank Memorial Fund Quarterly 149: 509–38.
Schindler, Y., and A. J. Scott. Forthcoming. “The Macroeconomic Impact of Chronic Diseases in the United Kingdom.” Journal of the Economics of Ageing.
Scott, A. J. 2024. The Longevity Imperative: How to Build a Healthier and More Productive Society to Support Our Longer Lives. New York: Basic Books.